When blood samples are stored the wrong way, hormone tests can give misleading results. AGEM researchers at the Amsterdam UMC Endocrine Laboratory found that renin, an important marker for diagnosing causes of high blood pressure, can appear falsely elevated if serum samples are stored at -20 °C. Their study also points to a simple fix: using special collection tubes with enzyme inhibitors, which prevent or even reverse the false rise in renin levels.
Ömer Özcan, PhD candidate at the Endocrine Laboratory noticed that renin concentrations were higher than expected in some blood samples that were stored at –20 °C. He suspected this happened due to a conformational change of prorenin into open prorenin at low temperature – also known as cryoactivation. This can cause falsely elevated levels of renin.
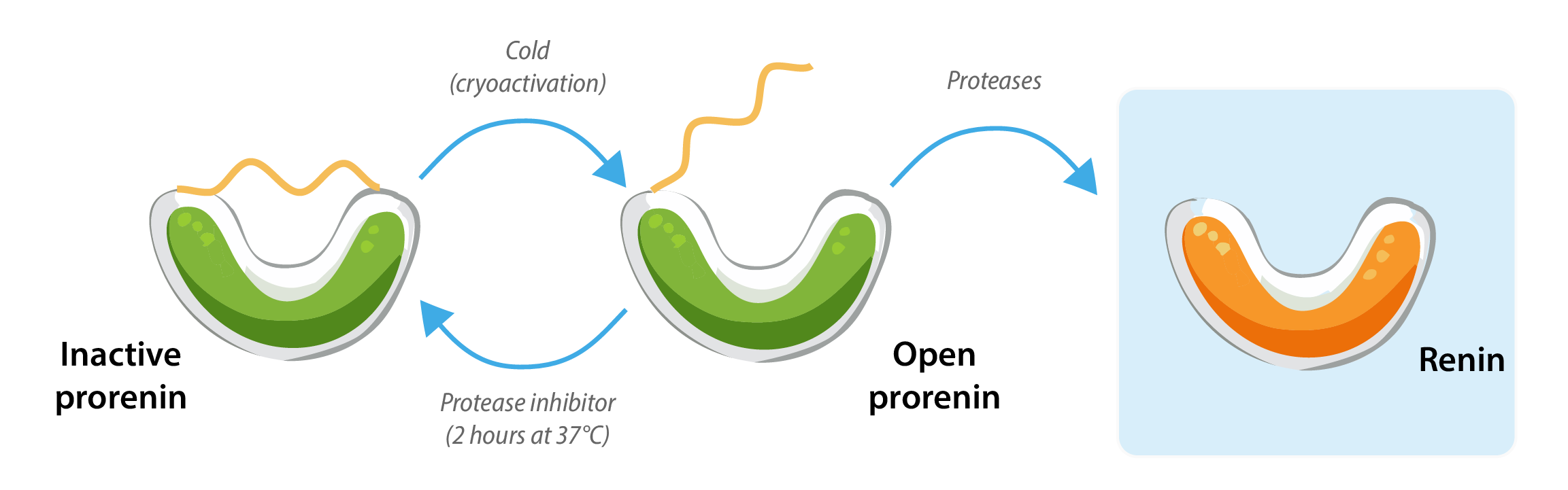 Diagram by: Barbara Verhaar (based on the diagram by Özcan)
Diagram by: Barbara Verhaar (based on the diagram by Özcan)
''This is a well-known phenomenon with samples that are kept between -5°C and +4°C, but these samples were stored in a –20°C freezer,” Özcan explains. This can have serious consequences in clinical practice, because renin is used as a marker to distinguish between different causes of high blood pressure.
Renin in medical practice
Doctors use renin levels to identify the mechanisms behind high blood pressure. “Renin levels are particularly important for diagnosing primary aldosteronism,” explains Professor Bert-Jan van den Born, internist in the vascular medicine department. “In my clinic, I often see patients whose blood pressure remains uncontrolled despite multiple antihypertensive drugs. Measuring both aldosterone and renin is essential: a high aldosterone-to-renin ratio indicates high aldosterone with suppressed renin. This can be caused by an adrenal adenoma that produces excess aldosterone.”
Primary aldosteronism is more common than many assume—affecting about 10 percent of patients with treatment-resistant hypertension. “If an adrenal adenoma is the cause, it can be surgically removed,” says Van den Born. “Afterwards, patients often see their blood pressure normalize and can reduce or even stop their medication.”
Frozen but not cold enough
Özcan and his colleagues wanted to figure out whether cryoactivation also occurs at -20°C and if they could reverse the cryoactivation process. To test this, several serum samples were stored at different temperatures, namely +4 °C, -80 °C and in two different -20 °C freezers.
As expected, there was no cryoactivation in samples stored at -80 °C, but there were high increases in renin concentrations in all other samples stored at different temperatures, including samples frozen at -20°C. Ozcan noted that the different -20°C freezers showed no significant differences in their effect on renin levels, ruling out factors dependent on freezer type. Likely, cryoactivation at -20 °C is not caused by storage at this temperature itself, but rather by the time it takes before the sample is completely frozen.
 Illustration by: Rosalie C. Martens
Illustration by: Rosalie C. Martens
A solution to cryoactivation
Although freezing at -80°C is safer, storing plasma samples at this temperature is not always feasible for smaller labs. Is there another way to prevent cryoactivation? Özcan investigated this by comparing serum stored in blood collection tubes that were coated with different protease inhibitors. Proteases usually cut prorenin into renin, and protease inhibitors prevent this cut from happening.
He defrosted the samples and remeasured the renin levels. After two hours at 37°C, renin concentrations had normalized in tubes coated with trypsin inhibitor. ''Honestly, we expected to see some change, but I was quite surprised by how effectively incubating the samples at 37°C in trypsin inhibitor tubes reversed the cryoactivation process.'' Trypsin is a known activator of prorenin, and this finding underscores its important role in the cryoactivation of prorenin.
It might also be a practical solution to the storage problem: using these tubes, serum can be stored at -20°C. ''This shows potential for other laboratories to store samples in a more convenient way without compromising renin test accuracy,'' says Annemieke Heijboer, professor in Clinical Chemistry, and last author of the study.
Authors
Rosalie C. Martens
Amber Mater
Barbara Verhaar
Science Communication Committee

