Researchers at Amsterdam UMC, in collaboration with colleagues at Harvard Boston, Crick Institute London and the University of Groningen, unraveled how the tuberculosis bacterium disables the patient's immune system. An existing drug appears to be able to prevent this process, so the tuberculosis infection can be treated. Amsterdam institute for Infection and Immunity researchers Sanne van der Niet and Nicole van der Wel were involved in this project, in this article they share the background, most important insights and their plans for the future.
Electron microscopy analysis (EM)
Sanne van der Niet: “The idea to study lipid accumulation in infected cells came from initial Electron microscopy (EM) analysis of cells infected with Mycobacterium tuberculosis." Sanne van der Niet and colleagues analysed the infected cells using an Electron Microscope which shows details of cells at nanometer resolution. Looking at these cells they noticed that when bacteria do not produce TbAd (a lipid only present in Mycobacteria) , these infected cells looked different compared to a normal infected cell. "We realized that lysosomes, the organelles responsible for breaking down particles and bacteria, are altered in mycobacteria-infected cells and that this change is due to lipid accumulation. This is an important finding because this could explain why cells are not able to kill tuberculosis bacilli effectively", Sanne van der Niet says. After this discovery, Harvard Medical School conducted Lipidomics, an analysis of all lipids, and confirmed the findings of Sanne van der Niet and colleagues.
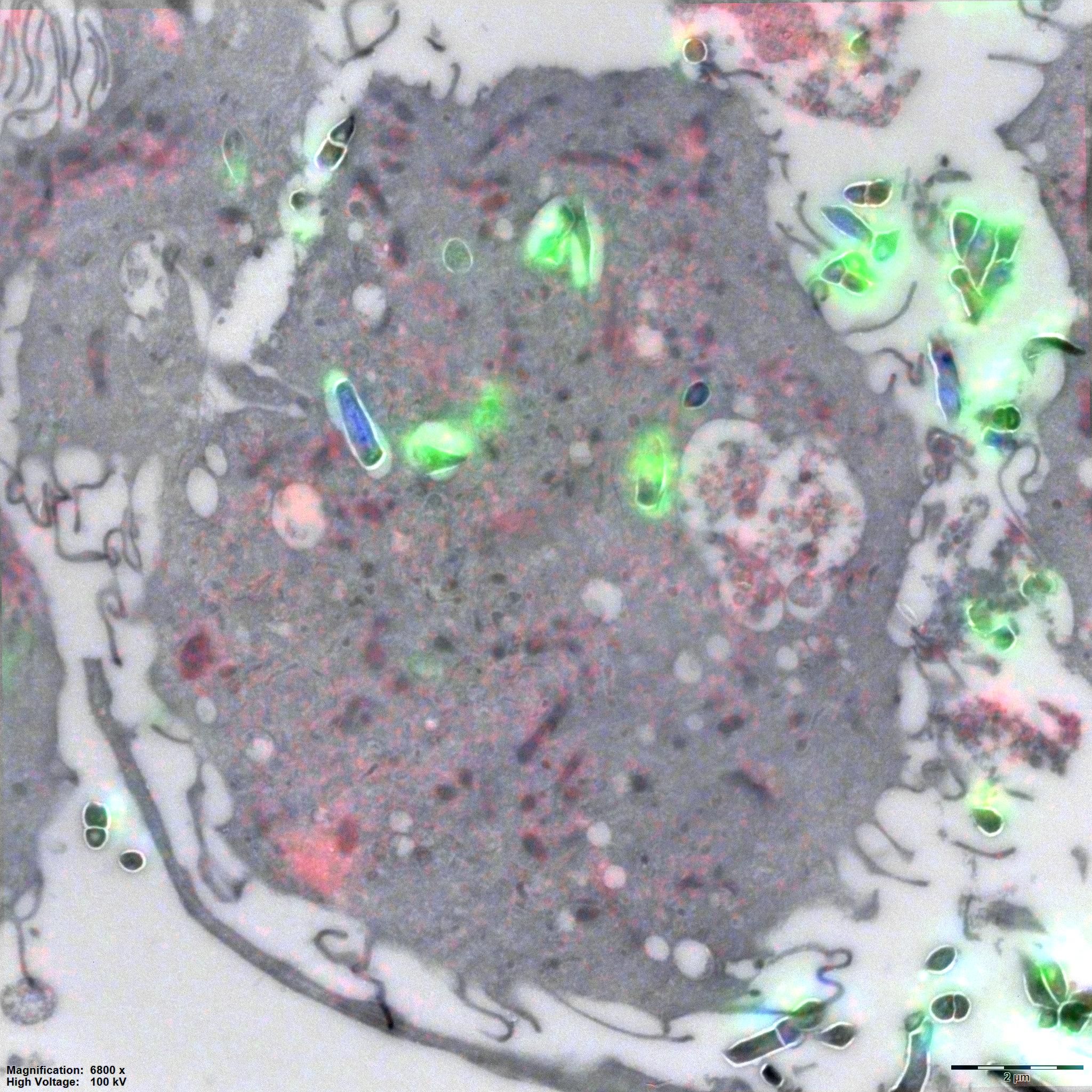 The figure shows a tuberculosis infected immune cell. A thin section of the infected immune cell was imaged using both a fluorescent microscope and thereafter an electron microscope. Images of both techniques are combined in this image, to indicate the localization of the bacteria in green, DNA in bleu and lipids in red.
The figure shows a tuberculosis infected immune cell. A thin section of the infected immune cell was imaged using both a fluorescent microscope and thereafter an electron microscope. Images of both techniques are combined in this image, to indicate the localization of the bacteria in green, DNA in bleu and lipids in red.
Is it possible to prevent the immune cells from storing fat?
This earlier research project, conducted by the partnership between Amsterdam UMC, Harvard and the University of Groningen showed that the tuberculosis bacterium produces large amounts of a substance not made by other related bacteria. This substance prevents the bacteria from being broken down by cells of the immune system. In a recent study, the researchers figured out why this is the case

by 23 collaborators from 7 different institutes, this provided an incredible exchange of knowledge and experience”.
Subsequently, in this follow-up research project, the researchers went looking for the Achilles' heel of the tuberculosis bacteria: is it possible to prevent the immune cells from storing fat? “We did this by using a drug developed against a similar process to treat Gaucher disease. This is a metabolic disease in which too much fat is stored in immune cells due to a mistake in a gene. Initial tests in the laboratory indicate that this drug does indeed appear to be effective and may offer a new way to treat tuberculosis” Nicole van der Wel shares.

Numerous possibilities for the future
This insight opened up a whole new insight in tuberculosis and a novel avenue for drug development. Interestingly the drugs arose from a surprising field: lysosomal storage diseases. This is exciting because the researchers found that two completely different diseases, an infection and a genetic disease share the same treatment. Therefore, they could learn a lot from lysosomal storage disease to better understand Mycobacterium tuberculosis (Mtb) infection.
Nicole van der Wel: “Following this research program we are going to test drugs related to the drug we discovered in our research project, to look for the most efficient drug candidate. Also preclinical follow-up studies started in collaboration with the National Institutes of Health (NIH) and Harvard Medical School.”
“We have a new Electron Microscope: the Talos 120, at the Electron Microscopy Centre Amsterdam. This high end microscope will be used for further, even more detailed analysis of cells affected by TbAd and Mtb infected cells. Previously, I was a PhD candidate at Amsterdam UMC, with this Electron microscope I will continue my work as a Post-doc with funding from NIH and Harvard Medical School”, Sanne van der Niet says.
For more information contact Sanne van der Niet or read the scientific publication.
Researchers involved
Sanne van der Niet, PhD Candidate Medical Biology at Amsterdam UMC
Nicole van der Wel, Head Electron Microscopy Center Amsterdam at Amsterdam UMC
Anita Grootemaat, Research technician at Amsterdam UMC
Funding
This work was supported by the National Institutes of Health (NIH) and Casma Therapeutics (Cambridge Massachusetts USA).
Text: Esmée Vesseur
Read our previously published articles about infectious diseases here:
In the future, cutaneous leishmaniasis will possibly be endemic in the Netherlands (December 2022)
Dormant cytomegalovirus (CMV) can lead to deafness in children (December 2022)
AII collaboration grant in 2020, ENW-M NWO grant in 2022: the story of Nicole and Coen (October 2022)

