"Not more, but fewer and more relevant alerts by a CDSS make such a system more valuable for healthcare providers and patients," says Amsterdam UMC's Professor of Medical Informatics Ameen Abu-Hanna, the study's principal investigator.
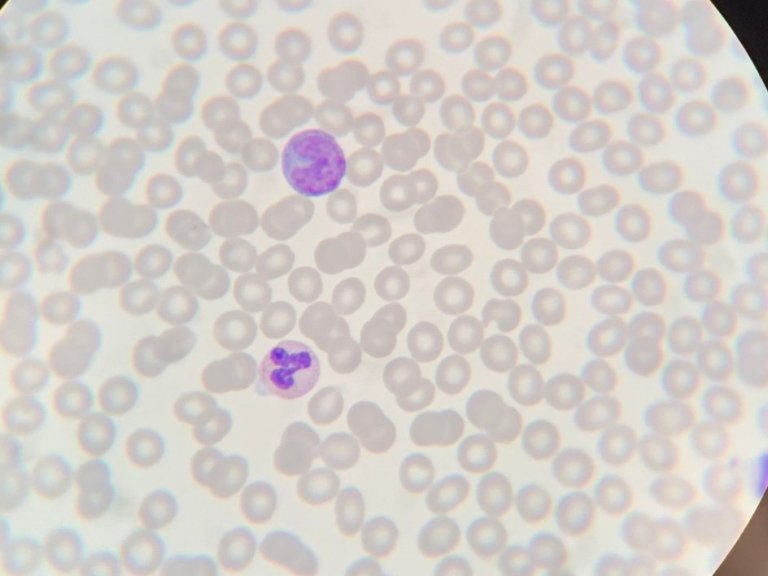
Combining two or more drugs at the same time can lead to either an increased effect or a reduced effect of the involved drugs. This may result in serious harm for patients. Drug combinations are more common in the ICU because ICU patients are seriously ill and, often, treated with many drugs at the same time.
Fewer, but more impactful alerts
CDSSs are used to alert ICU physicians about potentially risky drug combinations. These systems warn the physicians through alerts during drug prescribing. However, these systems are not properly tailored to the ICU environment, leading to an abundance of alerts that are not clinically relevant, which causes alert fatigue. Research shows that more than 80% of alerts for potentially risky drug combinations are dismissed by ICU physicians, including the important ones. This significantly diminishes the value of CDSS in daily clinical practice, and compromises patient safety.
"Patients in the ICU are critically ill and are often treated with concomitant drugs. At the same time, ICU patients are extensively and continuously monitored. Therefore, it is important to tailor the CDSS to the ICU environment to prevent alert fatigue and improve patient safety in the ICU," says Assistant Professor and co-author, Joanna Klopotowska.
Shorter stay in the ICU
Contrary to the current indiscriminate CDSSs, nine ICUs received during some period a CDSS that was carefully tailored to the ICU environment. This tailored system only showed alerts for drug combinations that were considered high-risk or needing extra monitoring, as defined by a national panel of ICU physicians and hospital pharmacists. The alerts for low-risk drug combinations were turned off. As a result of this adjustment, 12% fewer high-risk drug combinations were administered in the ICU patients, and the monitoring of possible side-effects pertaining to high-risk drug combinations was improved. Patients' stay in the ICU was also shortened.
This study shows that tailoring a CDSS to the ICU environment improves patient safety in the ICU patients. By alerting only where it matters, the ICU physicians were able to better recognise the dangerous drug combinations. This approach can also be valuable for other groups of patients such as neonatology, paediatrics and oncology. At the moment, many hospitals use CDSSs without customization to their specific patient groups, and the systems’ effectiveness is seldom scrutinised.
"We hope that our study inspires and stimulates hospitals to take a more critical look at all the alerts that healthcare providers receive through such systems. This will benefit patients and healthcare providers," says Klopotowska.
Low-Hanging Fruit
Even the ICU departments that did not participate in the study can easily adapt their CDSS today and make it more effective. These adjustments can be made manually in the existing systems and require minimal effort. To this end, the researchers have published two lists. A list of drug combinations that are high-risk in the ICU, for which alerts should be enabled, and a list of low-risk drug combinations that do not require alerts.
"Adapting ICU CDSSs is a low-hanging fruit that all ICUs in the Netherlands and beyond can benefit from, they do not have to reinvent the wheel for themselves." adds Tinka Bakker, at the time of the study the PhD candidate and co-author of the study. On the 7th of December 2023, she defended her thesis at the University of Amsterdam about tailoring the CDSS to the ICU environment.