McInnes, Professor of Rheumatology and Vice-Principal of the University of Glasgow will use his own anatomy lesson to map the molecule, just as Tulp mapped the arm all those years ago. A parallel which isn't lost on the Scottish professor:
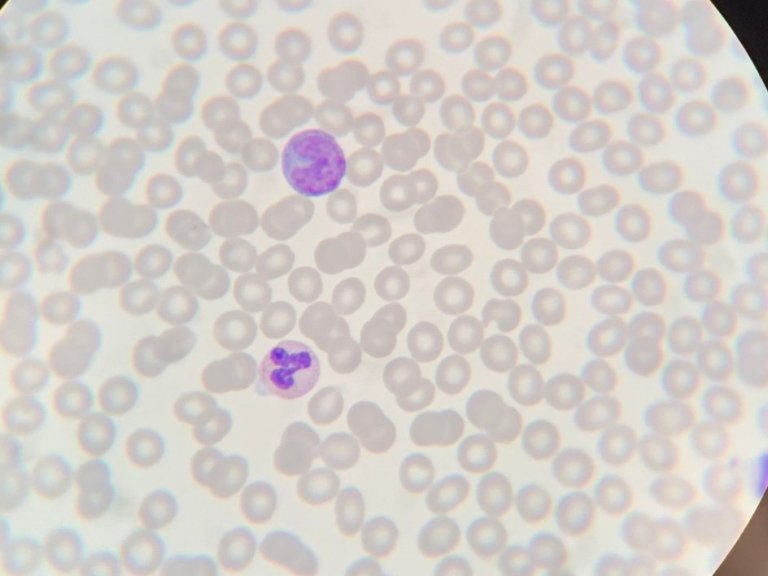
"Rembrandt's painting depicts macro-anatomy. Tulp is asking the fundamental questions: what are the structures under our skin? How do they function? And why are things not working? They were at the very cutting edge. We need to reconsider what a modern reinvention of the anatomy lesson might be. For me, we can do this by looking to molecular anatomy. By understanding where molecules and cells actually are in the tissue, their spatial orientation, we can start to learn extraordinary things about how diseases work.”
In Glasgow, McInnes applies molecular anatomy to one of the world's most burdensome conditions: arthritis. A condition with more than 100 variants that is estimated to affect the joints of more than 350 million people worldwide. The vast majority of those joints are affected by either osteoarthritis or rheumatoid arthritis, and it is the second, autoimmune condition, where McInnes dedicates most of his time.
Developmental Backwater
Rheumatoid arthritis is a lifelong condition that typically manifests itself in the joints but can also result in inflammation in the heart and in the lungs. This manifestation is driven by the body's immune system attacking itself:
"Millions are suffering because their immune system has diverted its attention from host defence to host damage inadvertently causing the destruction of the beautiful structures that make up our joints,” says McInnes.
While this process is clear to scientists many other aspects of the disease remain a mystery. Despite being first charted in a series of paintings by Paul Rubens in the early 1600s. Rembrandt's 17th century contemporary filled his paintings with figures whose hands depicted the symptoms of rheumatoid arthritis, swelling in the joints and deformation of the fingers.
It is believed that Rubens himself suffered from the condition and, just as his doctor would have explained then, the cause is unclear. It also remains to this today incurable. Nevertheless, the last twenty of the intervening 400 years have represented a "remarkable progress” in the world of rheumatoid arthritis:
"In terms of treatment, we've moved on from being a developmental backwater. Over a century, very little progress was made but in the last twenty years, remarkable progress has been made in understanding diseases of the joint," says McInnes.
Looking Deep Inside Ourselves
This "remarkable progress” is partly thanks to the advances in molecular anatomy that McInnes will speak about on the 16th of November. These advances have allowed for greater knowledge of the inside of the joint, facilitated by giant advances in the quality of imaging technology. Something what McInnes compares to leaps forward the telescope has made since it was in the hands of Galileo.
"A good way of thinking about this is to think in terms of telescopes. What Galileo was able to see in the 1600s, was not much more than blurry dots. And then telescopes evolved that were able start to discern distant and ever more distant galaxies. And now we send telescopes into space ever further away from Earth. The clearer the view, the more exquisite the sensitivity of the tool, the more we learn about where we are in the universe.
Precisely the same concept occurs when we look inside ourselves. And with modern molecular technologies, we can look deep inside ourselves, to the single molecular level and see how diseases are expressing themselves in a way that would have been simply awe inspiring for Tulp's attendees at the original anatomy lesson," reflects McInnes
This ability to see further, is something McInnes believes will help to solve the biggest stumbling block for the existing treatments against arthritis. Namely that whether or not a medication will work for a particular patient is still a guessing game for doctors. And even after this game, half of patients are still left without a working treatment.
"We need to move away from trial and error, we need to move to an eventual Nirvana where we understand the molecular composition of our patients in such a way that we can choose that perfect medicine at the right time. And give them that medicine before we get anything else," believes McInnes. This nirvana might not be so far away, mainly to due to the promise of the 'molecular scalpel:' a method of "using therapeutics to target the bad actor". However, unlike the scalpel Tulp wielded almost 400 years ago, McInnes’ works at level invisible to even Rembrandt's eye.
Molecular Scalpel
The work of the molecular equivalent of the scalpel begins with a tissue biopsy. This biopsied tissue is then treated with one of the myriads of possible treatments against arthritis. If this doesn't work, the present-day imaging techniques allow McInnes and his team to see why – on a molecular level. This facilitates an even greater understanding, allowing us to understand "what is and what is not the pivotal pathway in disease.”
However, the work of this scalpel doesn’t stop there. McInnes believes that by "molecularly dissecting disease" and understanding the 'pivotal pathways', we can create a snowball effect with enormous benefits for patients. Not only are patients presented with a personalised treatment plan for their own, distinctive variety of arthritis but scientists also learn lessons that they can apply to their next patient. A process that McInnes believes may be the key to allowing the field of rheumatoid arthritis to “dare to dream of finding a cure”.
"By combing the product of the lessons that we learn with each and every patient, we can develop new treatments and then we can treat biopsied tissue with the new treatment. This creates a cycle that allows us to dive deeper and deeper. This is the process that will lead eventually to long term remission for a majority of our patients, because we'll use the therapies to continuously inform us as to why they're working, or more importantly, why they didn't work," says McInnes.
Horses for Courses
Just as Tulp left his dissections behind to become the Mayor of Amsterdam, the Scot has also taken a detour. Although, unlike Tulp, McInnes wasn't prompted by political ambition but by a golf injury. A frozen shoulder, a stiff shoulder that can last for up to three years, left him unable to play golf, "heartbreaking," in his own words and shifted his attention, temporarily, from the joint to the tendon.
"It became very obvious to me, very quickly that the therapies that we have for human tendon disease, are very poor indeed. And so, we applied the same logic to human tendon disease, as had been applied in the preceding decade, to human joint disease," says McInnes.
While the joint, the meeting point of two bones supported by cartilage, has been explored and treatment improved by the use of antibody treatments, the tendon, which stabilises the joint was long forgotten due to a misplaced assumption.
"For 50 years, pathology textbooks had said that tendon diseases were caused by damage to, and the consequent structural failure of, the tissue. But after looking very carefully at early tendon disease we saw that it was an inflammatory condition and over the last seven or eight years, we have discovered the molecular and cellular pathways that lead to tendon disorders,” says McInnes.
In order to test this discovery, McInnes was forced to move outside of the lab and to another sport: horse racing, "it turns out that racehorses have a lot of tendon problems and, so, we actually began by treating tendons in horses by using a new medicine that we have discovered by charting our molecular map."
Molecular Anatomy Revolution
This medicine in now, among numerous others, part of a clinical trial ran from McInnes’ department in Glasgow, facilitating his own "return to the human.” A human in which rheumatoid arthritis increases the risk of heart attacks, strokes and depression. While the reasons for this are unclear, signs point to the same inflammatory pathways that drive the attack on the joints.
This presents are opportunity. By applying the molecular scalpel to other diseases, McInnes believes "this molecular anatomical revolution will be a way in which the disciplines finally come together to optimise outcomes for patients in the decades to come."
A level of curiosity and collaboration which McInnes is sure Tulp would have valued. "I think, sometimes we think of ourselves in the modern age as being the pinnacle of human curiosity but it's probably not true. Can you imagine how remarkable these guys were? The physicians in the Netherlands and other European countries in the 15th and 16th century, with extraordinarily blunt instruments by modern day standards, made remarkable clinical findings, many of which have stood the test of time.
This level of curiosity remains essential. We mustn't allow the technology to dazzle us, human ingenuity and curiosity are the essential tincture that will allow technology to transform lives,” concludes McInnes.