Accepting death can be hard, approximately 50% of people are afraid of dying, and discussions around the subject can be difficult for medical professionals but Pasman believes that it's time that we, as a society, give death room to be understood, discussed and, ultimately, accepted.
However, Pasman believes that the trend is moving in the other direction with more people, expecting to live longer and longer: "There are many more medical solutions nowadays, and you can live longer but not always with a good quality of life. People think that tlife can be engineered. I think it's human to think if there are medical possibilities, I should take those possibilities. And I think that it would be good to change that idea a bit. Life prolonging treatment can have side effects and time spent in hospitals can often use up precious time."
These expectations for a longer life are also being met, with the UN predicting that, by 2050, over 25% of the population in high-income countries will be over 65-years-old, more than three times the amount in 1950.
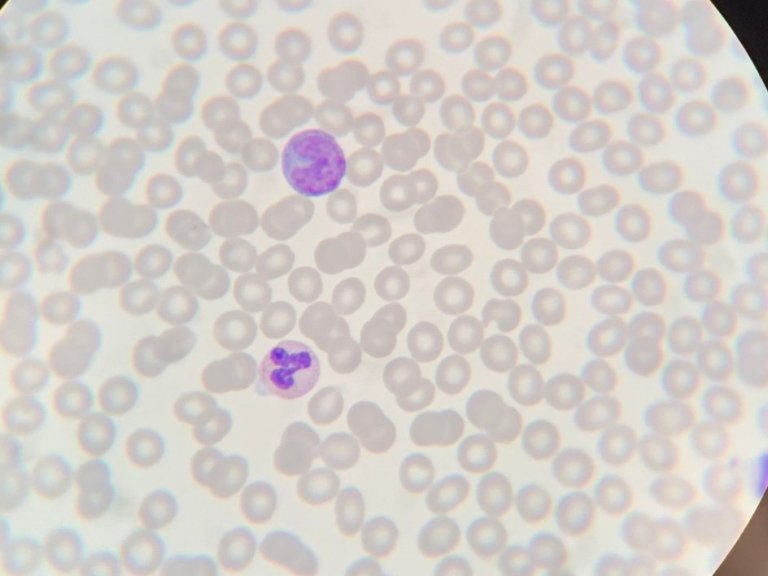
Nevertheless, extending life doesn't mean the people will stay healthy. With our current medical understanding, it's unlikely that life expectancy can exceed 95 and research also shows that age is the largest risk factor for cancer, neurodegeneration and the most common cardiovascular diseases.
In Pasman's eyes giving death a place in society can stimulate decision making and having a conversation about preferences and wishes at the end of life, in an Advance (alsosometimes called, Anticipatory) Care Plan (ACP). This makes the last part of life easier for both the person making the decisions and their family and friends. By having this conversation, people also have the chance to enjoy the last phase of their lives: "We need to stimulate people to think, what is important for me and what should I do now?”
ACP can have a number of benefits, both for the planner themselves but also for society. ACP can, naturally, increase the chances of dying in the desired place – for example, at home with family. Family, who in turn, experience less stress, anxiety and depression and who are more satisfied and have more understanding for their loved one's dying process.
With over 20 years of research experience, Pasman believes the empirical evidence is compelling, but her own experience of her father's death is a strong, anecdotal, case for the use of ACPs and, further, making the best out of the last phase of life: "My father died more than 10 years ago now. And he had cancer and it was really from the start there weren't any treatments anymore. And in a way, I was relieved. We left the doctor's office and then he said, Okay, there's one thing I want, I want to go with the whole family to the islands, like we did when you were young. And then I said, Okay, well, that's the first thing we are going to arrange now."
As mentioned above, these benefits, are not limited to the individual family but also extend, in the financial sense, to society as a collective. And while Pasman admits that "it always feels a bit weird to talk about money,” costs can rise rapidly. In her own research, Pasman and colleagues from the Amsterdam UMC have also found that costs vary depending on the cause of death and, indeed, the location.
Further studies, using British national data, have shown that costs increase the closer an individual comes to death, with this increase rising sharply in the final three months of life. This applies for all age groups, but increases the most, by more than 100%, for those over 90. Precisely the group who would most benefit from discussing their wishes.
One of these wishes can be about euthanasia. The Netherlands was the first country to permit euthanasia, in 1992, with a notification procedure, and the process was fully legalised in 2001. Currently, it is the cause of 4.5% of Dutch deaths and while this percentage has increased in the last twenty years, Pasman doesn't believe that euthanasia is a "solution for everyone” but rather something for a "small, small group of people.”
For Pasman, it's about moving from "survival mode” to thinking about "what is most important right now” and this shift applies to both patients and medical staff. Pasman recalls interviewing an oncologist, who regularly recommends drugs to terminal patients that can extend their lives. For some this is a fantastic solution which can allow them to make a trip like Pasman's father but Pasman believes that if these drugs, and many others like them, don't come with the question, "What do you want from the remaining part of your life?", then "death is being postponed, which is an easy decision but not always the best one."
Supporting people to make the best decision for them and their families is the ultimate aim of Pasman's research and to do this, there needs to be work in the community too. In order to speak to people and allow them to understand their options before they are already ill or approaching the end of life. In Pasman's view this is about "stimulating people to think about their end of life – to normalize it and make it part of life.”