Last June, Laura Cadenau, Infection Prevention expert, traveled to Suriname for the third time to support the health care system, hoping to bring the corona situation back under control.
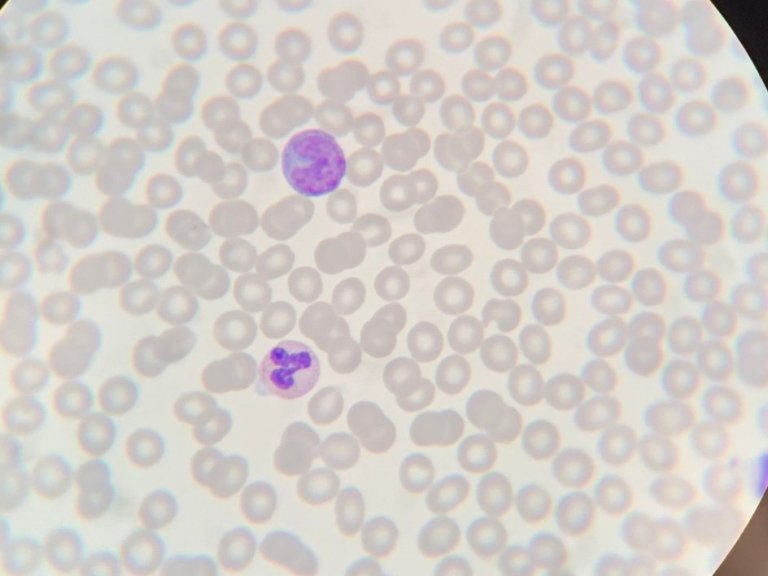
Absolutely indispensable behind the scenes, the Infection Prevention Department. This team makes every effort to prevent infections and the transmission of microorganisms such as bacteria, viruses and fungi in the hospital. "At Amsterdam UMC, we ensure that patients can stay in the hospital safely and that healthcare workers can also do their jobs safely," says Laura Cadenau, infection prevention expert. "Whether it's the MRSA bacteria, influenza or corona. That's our core mission."
Quest
When the first reports of a new virus arrived from China, her team was immediately on edge. "Because there were initially no clear guidelines for controlling this covid virus in humans, infection prevention was a pretty intense search," Cadenau says. "What do we do if patients also report here with the virus? How should we screen patients? What are the scale-up plans if it really becomes a pandemic? Which wards are suitable for cohort? What is the isolation policy? What personal protective equipment is necessary? And so on." In the period that followed, Cadenau and her colleagues discussed everything from disinfecting hands, air treatment in operating rooms, purchasing and inspecting protective equipment and advising healthcare personnel to contact investigations, setting up cohort departments and isolating patients.
"It was constant search for the right means to make the stay of patients and staff in the hospital as safe as possible. Definitely a challenge."
Suriname
When infection rates came down in the Netherlands in the summer of 2020, Cadenau could catch her breath. But instead of a well-deserved rest, she decided to travel to Suriname in her holiday to offer support in setting up and promoting infection control policies there as well. "On LinkedIn I saw a call from SU4SU (Surinamese for Suriname, ed.). Internist-Infectiologist Denise Telgt and her colleague, intensivist Jeroen Schouten of Radboud UMC were putting together a medical team. I reacted immediately. What else was I supposed to do? Twisting my thumbs in the Netherlands?." Shortly thereafter, she boarded the plane with a group of nurses, doctors, technicians and lab technicians.
Unimaginable
The infection policy that Cadenau had drawn up for Amsterdam UMC did not always prove to be of the same value in Suriname: "The options in Suriname are limited, so you have to improvise. In Amsterdam UMC, for example, we have an OR room that is only used for covid patients. But with a total of five ORs in one of the hospitals, they don't have that luxury there. They have to use those rooms continuously, for all types of patients. On top of that, they have little to no ventilation in those rooms. So what do you do with the aerosols in the air if a covid patient has just been operated on? One of the OR rooms turned out to have a window. Together we decided to operate on covid patients only in that OR room. After surgery, the window was opened for half an hour to refresh the air before bringing in the next patient, with or without covid. In the Netherlands, something like that would be unimaginable, but for Suriname it was the safest option at the time."
Risky situations
Cadenau was told by nurses from the Netherlands that healthcare workers sometimes reused protective equipment such as mouth masks and isolation aprons after a break and did not always wash their hands properly. "I provided training there on covid care and basic hygiene, but often there simply aren't enough protective materials on hand to grab a new set every time." That shortage of materials constantly creates dangerous situations. "For example, you have certain breathing tubes that, because of an increased risk of bacterial contamination of the patient, you are supposed to use once and replace after 48 hours. But the crisis in the hospitals in Suriname means there is not enough stock of those either. So we thought of a way to disinfect the tubes as best as possible and still use them again. With all the risks that entails. But necessity, no, disaster breaks the law. Without such a tube, the patient will die. There is simply no other option."
Improvise
From the healthcare workers in Suriname she has learned to be inventive and creative. "Scarcity is reality there, both in personnel and in needed medications and equipment. So improvising and coming up with alternatives is the order of the day. I have deep respect for how they do it." She has made friends for life. "Not only have I built up a very special bond with the medical team from the Netherlands, I have also been able to take many Surinamese people into my heart. An incredibly warm and hospitable people, despite the disaster that is now unfolding there."