The ear is often considered the epitome of a complex three-dimensional structure. In any case, it’s the shape that medical researchers all over the world like to conjure out of their 3D printers as proof of their inventiveness. So too in the laboratory of Arthur Bergen, Professor of Molecular Genetics, where the ear was one of the first objects that molecular biology post-doc Eszter Emri produced during a recent demonstration of their new 3D printer. As the print head shuttled delicately back and forth, the unmistakable form of a small, shiny white ear took shape in the petri dish.
But the finesse of this demonstration does not lie in the complexity of the shape, Emri asserts. “We have printed this ear using ordinary Nivea Cream,” she says, not without a touch of pride. “The art lies not so much in the shape as in the softness of the material we use. How do you prevent fluid material from simply running out of the printer? How can you control the water content needed to ensure the fluidity of some materials so that it evaporates at just the right moment? Those are the problems that occupy us in our experiments with 3D printing.”

Using stem cells as ink
The Nivea ear might impress the lay person, but the shapes that Emri is struggling with day in, day out are seemingly simple lines. “Recently we’ve been able to use stem cells as ‘ink’ in this 3D printer,” she explains. “A second breakthrough that made it possible to create a 3D print with living tissue is the unprecedented resolution we’ve achieved. We can now position cells with pinpoint precision, to within a couple of micrometers. We print them onto a matrix, a kind of mold of soluble synthetic polymers, for example. Later, we might be able to use cartilage. The idea is that the stem cells then grow into the desired cell type in an incubator.”
Printing structures for medical research
So much for the theory behind modern 3D printing with living tissue. In practice, many issues still need to be addressed. As Emri explains, “We are one of the few places in the world with such a hypermodern 3D printer in the lab. When we run into problems, there aren’t any instruction manuals telling us what to do, let alone a manufacturer’s helpdesk. We do have an excellent user group. Working with other users all over the world, we try to figure out how to print different structures and how to solve the problem of evaporation control and clear all the other practical obstacles along the way.”
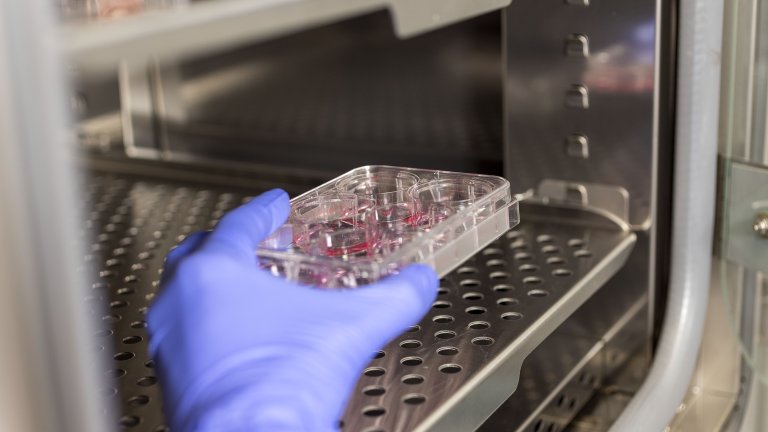
Meanwhile, the head of the department, Professor Bergen, is looking a step ahead. In collaboration with Theo Smit, Amsterdam UMC’s Professor of Translational Regenerative Medicine, he has set up a major project with the 3D printer at its heart. “3D printers have an enormous potential in medicine,” Bergen says. “Working with living tissue from the 3D printer can raise our fundamental research to the next level. We can also print solid, standardized structures for use in medical research, and ultimately we should even be able to make transplantable tissue.”
Macular degeneration
These days, Emri’s work also takes in these practical applications. For instance, she is currently attempting to print “drusen”: these are deposits that can accumulate in the eye as a result of age-related macular degeneration (AMD). They can be compared to plaques that build up in blood vessels and cause blockages in atherosclerosis.
Prof. Bergen fills in the background: “Macular degeneration is an eye condition that strikes 4% of people over 60 and up to 12% of people over 70. As drusen build up between the outer layer, the epithelium and the membrane of the retina, people slowly lose their vision. This ‘age-related blindness’ is a debilitating and progressive disease; it’s also one for which there are currently no effective treatments available. Macular degeneration is partly determined by your genes, but is also partly the result of unhealthy lifestyle choices such as smoking. Research into the disease is difficult because lab animals like mice don’t have a macula or ‘yellow spot’ on their retina as we do.” To better understand the progressive nature of blindness in the yellow spot, Bergen first wants to investigate how these drusen occur and accumulate. “Only when you understand how these structures form can you think rationally about treatments and preventive therapies.”
Before turning to the prevention of AMD, a different solution has appeared on the horizon. “We are already working on printing retinal tissue to replace areas that have been damaged,” Professor Smit reveals. “It’s possible to print both the epithelium and the underlying retinal cells using the patient’s own stem cells. In the US, fellow researchers have already received approval from the Food and Drug Administration to restore printed retinal tissue in lab animals. This application is not quite as futuristic as you might think.”
Text: Rob Buiter
Photos: Marieke de Lorijn