“It's very frustrating,” sighs Wouter de Jonge, Professor of Experimental Gastroenterology at Amsterdam UMC, “but we still don't know how Crohn's disease and other chronic intestinal disorders arise. Sometimes someone thinks they have found silver bullet, but it then turns out only to apply to small proportion of patients. We are gradually realizing that there can be a different cause in every patient suffering from inflammatory bowel disease (IBD).”
What the patients do have in common is a dysregulated immune response to bacteria in the gut. “The immune system flares up and can no longer be controlled. This has a negative effect on the mucous membrane lining the gastrointestinal tract. Special immune cells and aggressive immune substances then cause inflammation there. In the case of Crohn's disease, they also often occur elsewhere in the body, but it mainly manifests itself in flare-ups of severe abdominal pain, weight loss and diarrhoea with blood and mucus.”
Burden of disease
Although the cause may differ, certain factors seem to play a role: hereditary predisposition, diet, smoking, and the microbial composition in the gut. De Jonge: “The fact that we still know so little about the origins of IBD explains why current treatments have only limited success. More than 60 percent of patients with Crohn's disease do not respond to modern treatments that inhibit inflammatory proteins or immune cells. This results in an incomplete treatment of the disease, which can cause it to flare up. That can then lead to colon cancer or other complications that often need to be treated with surgery. It increases the burden of disease for the patient and also leads to high social costs. There is therefore an urgent need for treatments that are aimed at the individual patient. By using a test to determine in advance which treatment the patient will respond to best, we hope to enable more effective treatments.”
Unique rating
De Jonge, together with his colleague Geert D'Haens, Professor of Gastroenterology at Amsterdam UMC, will now lead the research into the development of such a predictive blood test. They were asked for research proposals in which solutions are devised for medicines that are often prescribed, but have limited effectiveness. With around 90,000 patients with IBD in the Netherlands, five million worldwide, and a multitude of patients with other inflammatory diseases such as rheumatoid arthritis and psoriasis, the research topic fitted seamlessly with the grant's theme. This was also apparent from the assessment that the application received: a top score of 15 out of 15. And as a result, 10 million euros.
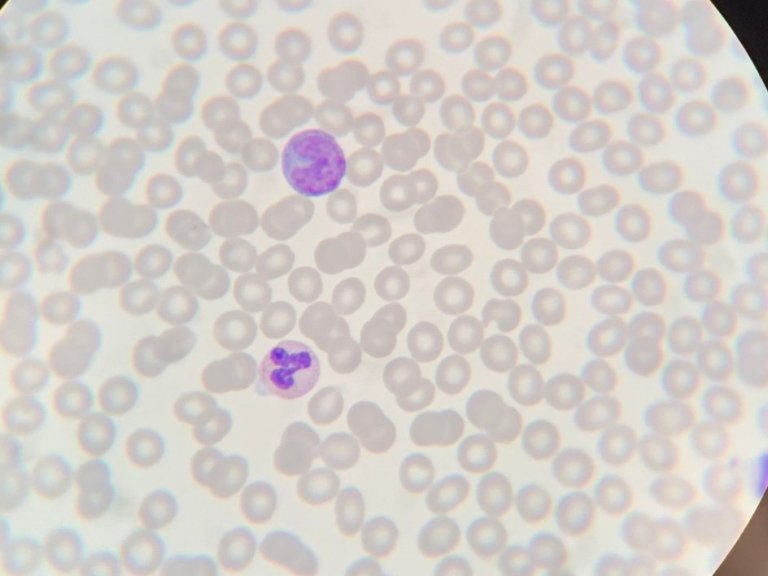
De Jonge: “In previous research, we had already done a lot of preliminary work together with the University of Oxford for the development of this test. For example, we had discovered specific epigenetic markers in the blood cells of IBD patients. So, we saw changes in the activity of certain genes without changing their genetic code. We did not find these markers in the blood of volunteers without the disease. We were then able to link a number of these markers to certain inflammatory genes associated with Crohn's disease. This in itself was a special find. We then investigated whether we could use these epigenetic markers in the blood to predict the response of a patient with Crohn's That turned out to be the case: by determining the DNA markers at the start of the treatment, we were able to predict which IBD patients would respond to the medication.”
New technique
By using machine learning to recognise patterns in a large amount of data, this finding could then form the basis of an algorithm. De Jonge: “It enabled us to develop a blood test based on a group of epigenetic markers that consistently differ in people who respond well to medication compared to people who do not respond. This so-called DNA methylation test was already available for cancer, but in that case, it concerns a marker on one piece of DNA. Our challenge was to test many more DNA markers at once, specific to each type of drug prescribed for Crohn's disease. We used a new technique for this, in which we unravel the DNA code per cell. In this way we can see where the DNA markings are located in each cell and which DNA markings lead to which gene expression. If, for example, a DNA marker is always accompanied by a response to a drug, then you know which gene is important. Once you get to the markers, you can predict whether a drug will work in Crohn's disease.”
Rapid test
With the European grant, the research group will test the blood test in a large clinical trial, spread over 52 centres in seven European countries. Half of these patients will be treated according to standard practice and from the other half, blood will be taken and sent to a central lab in Amsterdam UMC to be tested. This results in a pattern that fits one of the types of medication that are being investigated within this trial. The patient then also receives that therapy. De Jonge: “Ultimately, we want to know whether the test actually leads to more effective treatments. Exciting, because it is a completely new process for all of us. Incidentally, we also collect comparable data from patients with rheumatism or psoriasis. There is a lot of overlap in the syndromes; patients often suffer from a combination of these diseases. This means that we can use a blood test in the same way for these syndromes. This will then have an even greater impact on national healthcare, given the large number of patients suffering from rheumatism and psoriasis. Even in these diseases, the lasting effectiveness of the treatment is now often less than 50 percent.”
The research, says De Jonge, focuses mainly on determining biomarkers: “In blood, we are going to see which cells exactly carry which epigenetic marks, so that we understand which medicine improves the course of the disease. But we will also study, in the lab, how the disease develops in each patient. If our blood test results in not 40, but more than 60 percent of patients responding to the prescribed medication, then the test is successful. Then we just have to come up with something that improves the effectiveness of medicines themselves.”
This text originally appeared in Dutch in Amsterdam UMC's quarterly scientific magazine Janus.