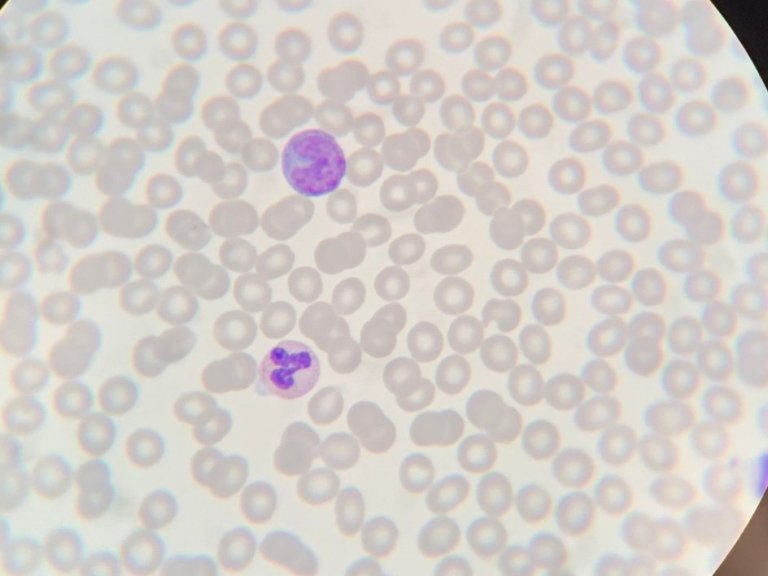
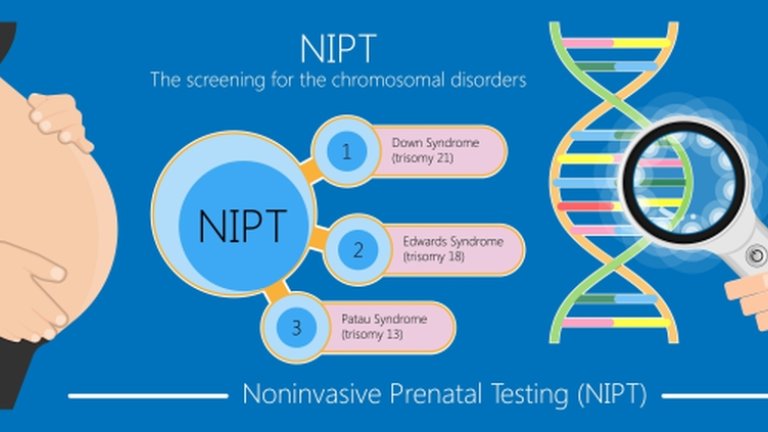
It’s quite straightforward, a simple blood test for the mother from the eleventh week of pregnancy onwards is all that is needed to determine whether her unborn child might potentially have Down’s syndrome, Edwards’ syndrome or Patau’s syndrome. “This test is based on a discovery dating back to the end of the nineteenth century”, explains Dr. Erik Sistermans, a Laboratory Specialist in Clinical Genetics at Amsterdam UMC. Dr. Sistermans also leads the national NIPT consortium, in which eight university medical centers and relevant professional associations cooperate on research into NIPT and on the development of this technique. “Way back then, it was already known that cells from the placenta were present in the mother’s blood. These are actually the unborn child’s own cells. By the 1940s, it had become clear that, in addition to these cells, the mother’s blood contains cell-free genetic material from the unborn child. At that time, however, science was not sufficiently advanced to exploit this information.”
Pieces of the puzzle
By the start of the new century, however, that had all changed. Assisted by Professor Cees Oudejans of the Department of Clinical Chemistry at what was then VUmc, Dennis Lo, a professor of Chemical Pathology from Hong Kong, found a way to interpret the traces left by the unborn child in its mother’s blood. Dr. Sistermans explains that “What you see in the blood are actually tiny pieces of DNA. A great deal of analytical processing and a powerful computer are required to analyze these pieces of the puzzle and obtain meaningful information from them. However, Lo and Oudejans were the first to use those puzzle pieces to find out whether an unborn child might potentially have three copies (trisomy) of chromosome 21, which causes Down’s syndrome, or of chromosomes 13 or 18, which give rise to Patau’s or Edwards’ syndromes, respectively.”
A bit frustrating
In 2011, the first commercial tests based on this new principle were launched on the international market. However, it was not until 2014 that the NIPT was officially introduced in the Netherlands. “That was a bit frustrating”, says Lidewij Henneman, professor of Patient Perspectives on Genetic Testing at Amsterdam UMC and co-director of the Amsterdam Reproduction and Development research institute. “The test was already commercially available in neighboring countries. Expectant Dutch couples had to travel to Belgium, for example, because here we were still developing official procedures in line with the Population Screening Act and other issues.”

Nevertheless, Prof. Henneman is keen to emphasize that she fully endorses these carefully considered procedures. “At the time, Amsterdam UMC led the way by cautiously introducing this test in the context of a trial. After all, countries are obliged to protect their citizens against any potentially adverse effects of screening. Indeed, it was with good reason that, in an article in the journal Nature, the American medical geneticist Professor Diana Bianchi (the ‘godmother’ of prenatal screening) cited the Netherlands as a textbook example of how to set up a carefully designed screening program.”
Major advantages of NIPT
Since 2014, the NIPT has been offered to any pregnant women who, based on the ‘old’ combined test, are at increased risk of having a child with Down’s syndrome, for example. This took place in the context of the TRIDENT-1 trial, which was led by Erik Sistermans. It soon became clear that the NIPT had major advantages over the combined test, which was still the standard test at that time. In the combined test, the risk that the unborn child might have a condition of this kind is assessed using the thickness of the nuchal translucency (a layer of fluid under the skin at the back of the neck, which is measured using an ultrasound scan), in combination with a blood test and the age of the mother. Those mothers who get a ‘positive’ result in either the combined test or the NIPT then have to undergo amniocentesis or chorionic villus sampling, to determine whether their unborn child actually does have Down’s syndrome. However, the latter tests involve an approximately 2 in 1,000 risk of miscarriage. That is, of course, a really terrifying prospect for expectant parents. Dr. Sistermans: “The evaluation of TRIDENT-1 showed that the combined test produces a large number of false alarms. With NIPT, however, this only happens in fewer than 1 in a 1,000 cases. Thus, the NIPT delivers a two thirds reduction in the number of risky and – in retrospect – unnecessary punctures.”

Informed choice
In 2017, following TRIDENT-1, Amsterdam UMC launched a follow-up trial in which any pregnant women in the Netherlands who wished to take this test were offered an opportunity to do so. That trial will run until April 2023. These days, very few combined tests are carried out, as more than 98% of couples who decide to use screening opt for the NIPT.Lidewij Henneman and Erik Sistermans still have a few key questions. Prof. Henneman: “One of the things I wonder about is why ‘only’ 46% of pregnant women in the Netherlands take part in screening. In Belgium, for example, that percentage is much higher. That may be partly related to the costs involved. The Belgian government charges pregnant women just €8 for the NIPT. In the Netherlands, the same test costs €175! A recent Dutch study showed that women from deprived areas are less than half as likely to opt for an NIPT than women who live elsewhere. An alternative explanation for the relatively low national screening level might be that we, in the Netherlands, tend to take a more positive view of people with Down’s syndrome. It might also be due to the carefully considered way in which screening is offered here, and to the associated counseling process. Thus, we and our researchers want to explore people’s reasons for deciding whether or not to take part in screening, and the extent to which pregnant women are making an informed choice.”

Barrier
The influence of counseling should not be overestimated. At least, that is the view of Eva Pajkrt, professor of Obstetrics at Amsterdam UMC. “In the Netherlands, very high quality prenatal counseling is available throughout pregnancy. At the same time, many parents already have a clear idea of what they want when they first contact us.”The research carried out by Prof. Pajkrt and her colleagues focused on women’s reasons for deciding whether or not to take part in screening. “In 2007, when the government first started charging for the combined test, there was a drastic decline in participation levels. That’s why I believe that the government’s current €175 charge for the NIPT could be a major barrier for a substantial proportion of women. This is especially true of relatively young mothers, who may feel that they are unlikely to have a child with Down’s syndrome. In cases such as these, the parents often prefer to avoid that expense.”Pajkrt also feels that the government’s decision to charge for the NIPT is unintentionally sending the wrong message. “What you are really saying here is, ‘We don’t think that this is important enough for us to offer it free of charge.’ It seems odd that, during this COVID-19 pandemic, anyone who wants to go to a festival can get a free test, while those seeking prenatal screening during pregnancy have to pay a significant part of the cost themselves.”
Watch the video on the prenatal test NIPT
Tests for deafness
As the chair of the national NIPT consortium, Erik Sistermans is already exploring a range of options that go beyond the current NIPT. “In the Netherlands, this form of prenatal screening is coordinated by our consortium, with support from the Ministry of Health, Welfare and Sport and the Netherlands Organisation for Health Research and Development, which funds health research. This national partnership is not only very important, it is also highly effective. For instance, together with our counterparts at Radboud UMC in Nijmegen, we are already exploring the options for using the NIPT to detect traces of cytomegalovirus. In children, this can lead to congenital deafness and various other abnormalities. Furthermore, the examination of specific fragments of RNA in the NIPT may help us to identify another risk to mother and child – pregnancy-induced hypertension and toxemia, also known as preeclampsia. In a 2020 trial among 161 pregnant women, it was found that a modified form of the NIPT was able to correctly predict – in the first trimester of pregnancy – that four of these subjects would go on to develop preeclampsia in their second or third trimester." We now want to validate this technique on a larger scale.
Dr. Sistermans and Prof. Henneman expect the range of conditions that can be detected using the NIPT to gradually expand. “As before, we will use the NIPT consortium’s multidisciplinary approach to provide this service, in a carefully considered way, to expectant parents.”