There are eight billion people living on this earth, each of us unique. When people get sick, the disease process and disease pattern is different for each individual. Gender, age, weight, height, history and genetic profile are among the many factors that influence this. Every individual is different, but not in terms of antibiotic dosage. Patients around the world receive the same dosage of antibiotics. This tactic is justifiable for patients who have mild symptoms; after all, this standard dosage was chosen for a reason. However, too many antibiotics can be toxic and too few antibiotics can lead to unsucessful treatment in those with severe infections or sepsis. There must be a better way, in Paul Elbers’ eyes. And so together with his team he sought to integrate a bedside decision support software called AutoKinetics into the Electronic Health Record (EHR) to optimize antibiotic administration in the Intensive Care Unit (ICU).
Dr. Elbers: "Through our decision support software, healthcare professionals in the ICU can see in the EHR how much antibiotics, according to the software, are currently in the patient's blood and how much this will be in the future if the current dosage is continued. This allows one to clearly see when the antibiotic concentration goes outside the ideal values, the software can then calculate what needs to be administered to get to the ideal value. It is a bedside, real-time, data-driven and personalized system for antibiotic dosage."
From byte to bedside
Developing this decision support software did not happen overnight. "The whole process took five years. But we are very proud of it: it was developed entirely within the walls of Amsterdam UMC. We distinguish ourselves with this research because we really do everything ‘from byte to bedside’. We arranged everything regarding the documentation and legislation, creating the model, the drugs, developing the software, storing the data, dosing the drugs and implementation into the clinic” says Dr. Elbers.
The research took place entirely within Amsterdam UMC and involved three research institutes. Amsterdam Institute for Infection and Immunity (AII) due to the focus on sepsis and septic shock in this study. Amsterdam Cardiovascular Sciences (ACS), since at the ICU traditionally the focus is on the heart and blood circulation. Amsterdam Public Health (APH) since within APH they focus on digital health, a research direction into which the developed AutoKinetics software fits perfectly. The following Amsterdam UMC researchers were involved: Paul Elbers, Tingjie Guo, Reinier van Hest, Ron Mathot, Eleonora Swart, Armand Girbes, Lucas Fleuren, Patrick Thoral, Harm-Jan de Grooth, Luca Roggeveen, and Ronald Driessen. Furthermore, two OLVG researchers were involved, Bas van den Bogaard and Rob Bosman.
From 3 to 69 percent
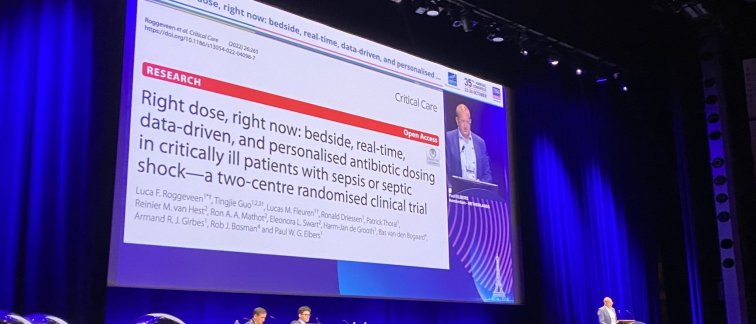
The goal of Paul Elbers and colleagues was to include at least 300 patients, COVID-19 hindered this. Dr. Elbers: "We did manage to include 252 patients. Our study was a two-centre Randomized Controlled Trial (RCT), this means that of the physicians of these 252 participants, half were exposed to the 24/7 decision support software, the other half did not receive this decision support software, these patients received the standard antibiotic dosage. Within our study we looked at four antibiotics: vancomycin, ciprofloxacin, meropenem, and ceftriaxone."
The primary outcome measure of the study by Paul Elbers and colleagues shows that the desired antibiotic concentration is achieved with AutoKinetics. In particular, the AutoKinetics software had an impact on the antibiotic ciprofloxacin. In the ciprofloxacin intervention group, the desired antibiotic concentration was achieved within 24 hours in 69% of cases versus 3% in the treatment as usual condition. For the other three antibiotics, Paul Elbers and colleagues found no differences between AutoKinetics and treatment as usual in clinical outcome measures. Possible explanations are that it was already administered at a good level in the treatment as usual condition or that the group size did not have sufficient power to find significant results.
Physicians receptive to AutoKinetics use
One of the key insights for Paul Elbers is the finding that physicians are open to using the decision support software. Paul Elbers: "Physicians in the experimental condition, who were exposed to the AutoKinetics software, were always presented with the choice of applying the advice of AutoKinetics or ignoring it. Only in 2% of the patients the advice was not followed and dosage was administered according to the standard guidelines, in 98% the AutoKinetics advice was followed."
What healthcare professionals thought of AutoKinetics has not been systematically researched. Paul Elbers: "However, what I have heard personally is that healthcare professionals liked the advice of AutoKinetics, mainly concerning the graphical display I have heard positive sounds, colleagues had confidence in the program. What I have heard from colleagues over the years and experienced myself is that correct dosing of antibiotics is extremely precise, it is mathematically very difficult, therefore a program like AutoKinetics is more than welcome."
What will the future hold?
As indicated by Paul Elbers, AutoKinetics advice was deviated from in only 2% of cases. This shows that physicians are open to this form of technology. Paul Elbers: "What is important here is that this decision support software has now been developed, for us it is reasonably easy to apply this software to other healthcare challenges. The recently developed Pacmed Critical discharge software is a good example of this."
Paul Elbers and colleagues have the ambition to build on the above insights in follow-up research and are therefore talking to a number of commercial parties for the further development of AutoKinetics. Even though this has so far been done entirely within the Amsterdam UMC, this is unfortunately not possible for further development. Dr. Elbers: "While we have been working on this software for the past five years, the 'Medical Device Regulation' came into effect in May 2021. One has to comply with this regulation when working on new medical devices. Technically, with this new regulation, it is still possible for an academic hospital to develop its own software, but this requires a quality system with thorough maintenance that goes beyond the capabilities of a hospital. The investment for this is better borne by commercial companies. This is why we are currently meeting with companies to share our knowledge and continue working together on the AutoKinetics research."
In addition, ICUdata is a recent initiative that Paul Elbers and colleagues founded, for which they received a grant of 2 million euros from the Dutch Association of Healthcare Insurers. Within this software, all data from Intensive Care Units in the Netherlands is combined. This has several advantages: the dataset is much larger and because differences in treatment exist between the hospitals in the Netherlands, follow-up research can also look at a possible contribution of those differences to treatment. The pioneering hospitals participating in this study are: Erasmus MC, OLVG, Medisch Centrum Leeuwarden and Amsterdam UMC.
Artificial Intelligence should be included into the schooling of healthcare professionals
Paul Elbers sees an important task for education to sufficiently introduce young doctors and nurses to data, its benefits and risks in their training. Paul Elbers: "What I hope for the future is that young doctors and nurses become more aware of the possibilities and risks of using Artificial Intelligence in medicine. The use of data will become increasingly important to cure patients in the future. I notice that this is not yet sufficiently prevalent among young healthcare professionals. It is important that we take action. I expect new positions such as physician data scientist to emerge in the future."
To contribute to this himself, Paul Elbers is a member of the Amsterdam Medical Data Science community. An association of 2,000 data scientists, academics, business professionals, doctors and nurses in the Amsterdam metropolitan area. The goal of this
community is to connect healthcare and data science.
For more information contact Dr. Paul Elbers or read the scientific article here.
Text: Esmée Vesseur
Curious to learn more about our Artificial Intelligence research? Read our recently published articles:
Data of ICU patients can answer thousands of questions (April 2022)
Groundbreaking: Artificial intelligence supports ICU physicians in patient discharge decision (August 2022)