Mitochondria are very small organs in cells that use oxygen to make energy. Until now it was thought that cancer cells avoid using those 'energy factories'. “From our research we now know that the oesophageal cancer cells that do use mitochondria to make more oxygen and thus arm themselves against radiotherapy,” says researcher Amber van der Zalm. “The cancer cells create more energy and can repair the damage from the radiation. This means that the radiotherapy has less chance of killing the cells.”
Radiation not always effective
Currently, patients with oesophageal cancer whose tumour is to be surgically removed first receive a treatment with chemotherapy and radiotherapy. This study makes clear why the effectiveness of this pre-treatment leaves something to be desired in many patients. “We believe this study is an important contribution to improving the treatment of oesophageal cancer. And possibly also for other tumours that are irradiated," says researcher Mark Dings.
Improve the effect of radiation
There are drugs that can counteract the production of mitochondria in the cancer cells. In the laboratory, one of these drugs greatly improved the effectiveness of radiotherapy. Not only were the tumour cells more inhibited in their growth, their ability to regrow after stopping treatment was also prevented. Because radiotherapy is often given in a targeted manner, its harmfulness can also be limited to the region around the tumour. This lowers the patient's risk of adverse side effects. The researchers are now looking at whether they can set up a clinical study to further map these effects.
Honoured on the front page
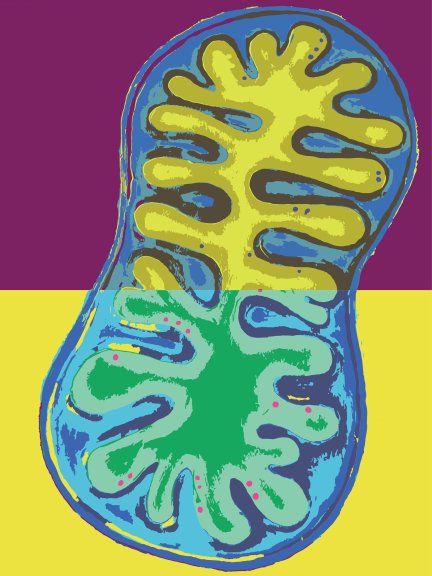
The scientific journal Cell Reports Medicine selected this study for its front page. First co-author Amber van der Zalm made an acrylic painting of a mitochondrion. Together with co-author Tatum van Maanen, they made a digitized, colour-adjusted version (see cover photo).
Oesophageal cancer is currently the seventh most common cancer in the world and effects more than 500,000 people each year. The study was funded by the KWF Dutch Cancer Society and the ONCODE institute.

