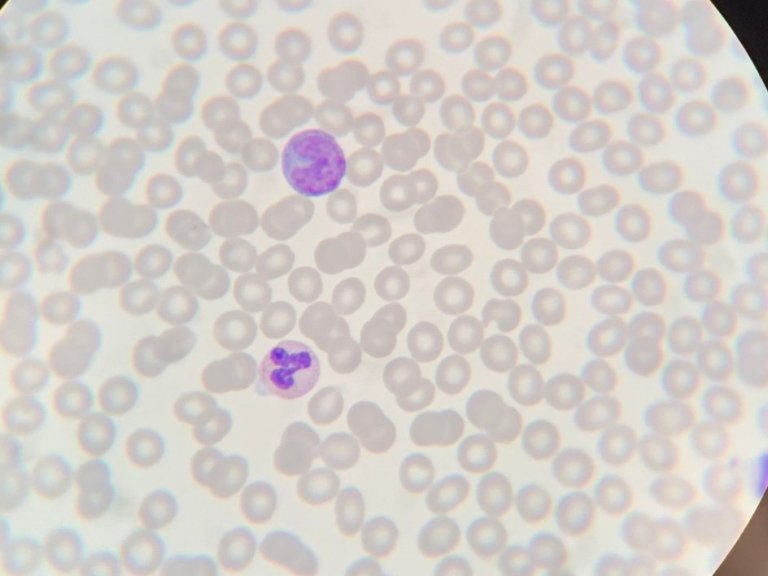
Research at Amsterdam UMC in recent years has contributed greatly to a better understanding of the biology of the disease. This study, the largest ever conducted in CLL, with a younger and fitter patient group builds upon these findings. CLL originates in B cells, a type of white blood cell that produces antibodies against bacteria and viruses. Therefore, one of the most common complications of this disease are, often severe, infections.
Previously it was believed that these CLLS were very difficult to kill. However, research revealed this not to be the case, granting researchers access to a raft of new treatment options. Arnon Kater, professor of haematology at Amsterdam UMC and chair of the HOVON CLL study group, explains that “just like a Formula 1 car on the track, we saw that the CLL cells in the blood are very vulnerable.
The protein Bcl-2 protects cells from dying in the blood. This protection gives the cells time to go for a pit stop, just like a Formula 1 car. The pit stop is the lymph node where the cancer cells can recharge and then divide.”
The researchers learned from previous studies that the drug venetoclax effectively inhibits the Bcl-2 protein. Cells in the blood do still die but, crucially, not during the pit stop in the lymph node. "By combining venetoclax with drugs that can do their job within the pit lane, we thought that combinations were possible that were debilitating and would be more effective than chemotherapy," says Kater.
Largest study to date
The phase 3 randomised trial, also known as the GAIA/CLL13 trial, was conducted with a total of 920 fit patients with CLL in 159 hospitals in 9 European countries and Israel. About a quarter of the patients came from the Netherlands. The patients were placed in four groups and received either chemotherapy and an antibody (standard treatment), or the drug venetoclax in combination with an antibody (either rituximab or obinutuzumab). The fourth group received ventoclax, obinutuzumab and the specific kinase inhibitor ibrutinib. Importantly, in all four groups, the treatment was temporary, in contrast to earlier studies that continued either venetoclax or ibrutinib, which prolongs exposure to side-effects, dramatically increases the costs and inevitably results in development of resistance.
All groups with venetoclax had fewer side effects, and that the combinations of venetoclax with obinutuzumab were more beneficial than the standard treatment with chemotherapy. Treatment was specifically discontinued in patients with an aggressive form of the disease (so-called IGHV unmutated variant, which resolves in 50% of patients). On average, after 3 years in the more aggressive disease group, in 35% of those who received chemotherapy, the disease had returned. For those who received the experimental combination therapy, this was only 18%. Making the combination therapy twice as effective for this group.
Benefits of combination therapy
Until now, chemo-immunotherapy has been the most effective treatment for patients with treatment continuing indefinitely. With drug-combination therapy it is now possible to stop treatment after a year.
“This study shows that with clever temporary and safe combinations, you can allow patients to be treatment free in the long-term, with a much lower chance of developing resistance.
And we also think that it is even possible to stop the combination therapy earlier than after a year. We now want to investigate this,” says Kater. This not only reduces side effects, but also healthcare costs.