Over the past decade, HIV care for transgender women* in the Netherlands has improved, with more individuals being linked to care and achieving viral suppression. This was demonstrated in an 11-year study by researchers from The Amsterdam Institute for Immunology and Infectious diseases (AI&I), Public Health Services (GGD) Amsterdam, Stichting HIV Monitoring (SHM), The Amsterdam Public Health Research Institute (APH) and the Amsterdam Institute for Global Health and Development (AIGHD). Despite this progress, challenges persist, such as late HIV diagnosis and the fact that less than 90% of transgender women consistently achieved viral suppression.
Research led by Dr. Jongen and colleagues examined the HIV care continuum among transgender women in the Netherlands from 2011 to 2021. The study found that fewer than 90% of transgender women linked to care were virally suppressed, and late presentation at the time of diagnosis was common.
Increase in Transgender Women Linked to HIV Care
Over time, the number of transgender women linked to care increased from 104 in 2011 to 239 in 2021. The majority of transgender women who were linked to care, were retained in care, received Antiretroviral Therapy (ART) and were virally suppressed during this period. However, the proportion of women who had an undetectable viral load was below 90% each year.
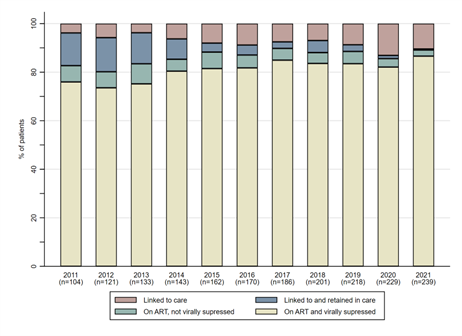 Figure 1. Retention in care, ART use and viral suppression among transgender women who were linked to care between 2011 and 2021, the Netherlands
Figure 1. Retention in care, ART use and viral suppression among transgender women who were linked to care between 2011 and 2021, the Netherlands
Late Presentation in Newly Diagnosed Transgender Women
The study also revealed that late presentation is prevalent among transgender women newly diagnosed with HIV, with 0% to 33% presenting with AIDS at diagnosis between 2011 and 2021. For comparison, in 2022 in the Netherlands, 122 individuals (32%) were diagnosed with advanced-stage HIV infection, which is defined as having a CD4 count below 200 cells/mm³ or being diagnosed with AIDS. This group included 44 men who have sex with men (MSM) (21%), 45 other men (48%), 31 women (45%), and 2 transgender men and women (15%).
What is Viral Suppression in HIV?
Viral suppression refers to reducing HIV levels in the blood to very low amounts (below 200 copies per milliliter) through consistent ART use. This helps protect the immune system, prevent AIDS, and minimize the risk of HIV transmission. Achieving viral suppression is a key goal of HIV treatment.
Data Collection and Demographic Overview from the ATHENA Cohort
Data for this research was drawn from the ATHENA cohort, maintained by the Stichting HIV Monitoring, which captures demographic, treatment, and HIV-related information from approximately 98% of individuals in care. Key demographic data collected at enrollment include year of birth, country of birth, sex assigned at birth, gender identity, and likely transmission route of HIV. Since 2015, gender identity has been recorded, with adjustments made for transgender individuals. Data on HIV diagnosis, ART use, and the occurrence of AIDS-defining conditions are gathered from clinical visits and imported directly into the ATHENA database, ensuring comprehensive monitoring of health outcomes.
Addressing Barriers to Improve HIV Outcomes
To improve outcomes, efforts must focus on identifying barriers to early HIV diagnosis and optimizing care for transgender women. Collaborating with the transgender community to design targeted interventions will be essential for improving retention in care and achieving better HIV outcomes.
An important collaborator in this initiative is the Trans United Clinic (TransKliniek), which specializes in healthcare for transgender and gender-diverse individuals, addressing their unique medical and psychological needs. Located in Amsterdam and Utrecht, the clinic provides comprehensive assessments, hormone therapy, and support for surgical procedures. Through collaboration with various healthcare professionals, the clinic aims to improve access to quality healthcare for the transgender community. However, it currently faces financial and logistical challenges that hinder its ability to provide HIV care and treatment. Both clinics operate with limited capacity, affecting their ability to meet growing demand. In response, Dr. Jongen and colleagues are actively seeking grants to enhance access to HIV prevention and improve care interventions.

For more information contact Vita Jongen (v.w.jongen@amsterdamumc.nl) or read the scientific publication below:
Researchers involved
V.W. Jongen1,2,4, PhD, Postdoc researcher
C. Daans1, MD
A.I. van Sighem2, PhD, Senior researcher
M.F. Schim van der Loeff1,3,4,5, Professor of epidemiology of sexually transmitted infections
K. Hage1,4, MSc, PhD candidate
C.A.H. Welling1, MD, Physician in training for Sexologist
A. von Vaupel-Klein1,6, MSc, Medical Doctor
M. den Heijer7,8, Professor of Endocrinology
E.J.G. Peters4,7, PhD, Internist-Infectious Diseases and Acute Medicine Specialist
M. van der Valk2,3, 4, Professor of Internal Medicine
P. Reiss2,3,5,9,10, Professor of Medicine
M. Prins1,3,4,5, Professor of Public Health
E. Hoornenborg1,3,4,5, PhD, Principle investigator
on behalf of the ATHENA observational HIV cohort
1Department of Infectious Diseases, Public Health Service Amsterdam, Amsterdam, The Netherlands
2Stichting hiv monitoring, Amsterdam, the Netherlands
3Amsterdam UMC, University of Amsterdam, Internal Medicine, Amsterdam, The Netherlands
4Amsterdam Institute for Immunology and Infectious diseases (AI&I), Amsterdam, the Netherlands
5Amsterdam Public Health Research Institute (APH), Amsterdam, the Netherlands
6Trans United Europe, Amsterdam, the Netherlands
7Amsterdam UMC, Vrije Universiteit Amsterdam, Internal Medicine, Amsterdam, the Netherlands
8Center of Expertise on Gender Dysphoria, Amsterdam UMC, VU University Medical Center, Amsterdam, the Netherlands
9Amsterdam UMC, University of Amsterdam, Global Health, Amsterdam, the Netherlands
10Amsterdam Institute for Global Health and Development, Amsterdam, The Netherlands
Funding
The ATHENA Cohort is managed by the Stichting HIV Monitoring and is funded by the Dutch Ministry of Health, Welfare and Sport through a grant from the Centre for Infectious Disease Control at the National Institute for Public Health and the Environment.
*Definition transgender woman used for this study: Woman who was assigned male at birth yet identified as woman during time of study. The transgender woman can but does not need to have completed medical transition in order to identify as women.
Learn more about the collaborative HIV research of Stichting HIV Monitoring and the Amsterdam institute for Immunology and Infectious diseases:
Despite access, one-third of people with HIV and hepatitis C (HCV) not treated for HCV (April 2023)
Improved survival by screening for anal cancer precursors in people with HIV (January 2023)
Text: Esmée Vesseur

